By the bioMérieux Connection Editors
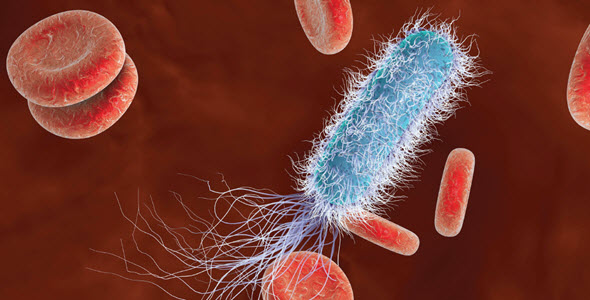
Sepsis is widespread and deadly, affecting 49 million and killing 11 million people worldwide each year. Early treatment of sepsis has been shown to improve clinical outcomes—and inversely, delays in treatment have been shown to lead to higher risk of patient death.
However, treatment must also be appropriate for the underlying infection. Because of that, advancements in diagnostic speed, range, and accuracy are critical for addressing the continued rise in sepsis cases and deaths. The ability to assess sepsis risk and confirm whether the initial, empiric therapy is ideal for the patient can help save lives while contributing to antimicrobial stewardship.
Antibiotic resistant infections and multi-drug resistant infections have been on the rise in recent years. When it comes to sepsis, these infections have the potential to be much more dangerous because they can be difficult to treat. Quickly identifying the infection and which antibiotics it is susceptible to helps physicians select the optimal treatment for the patient.
Advances in Blood Culture & PCR Technology
There are a range of ways to identify infections, from traditional culture and manual methods to more recent automated methods. In many cases, the speed of blood culture is a limiting factor in time to diagnosis, so newer blood culture tools and systems that improve turnaround time can make a difference. Although blood culture is considered the gold standard for identification of pathogens, it cannot detect every type of infection because some microbes do not readily grow in a culture environment.
While blood culture remains a critically important diagnostic tool regardless of its limitations, polymerase chain reaction (PCR) techniques can help fill some of the gaps. PCR offers significant advantages in speed for specific types of pathogens and can test for a range of infections all at the same time. This can be especially helpful for patients with complex infections involving multiple pathogens.
Achieving Better Patient Outcomes for Sepsis While Reducing Antibiotic Overuse
There are ways that physicians can achieve better outcomes for their patients using currently available technologies and sepsis protocols. Preliminary sepsis risk assessment and monitoring patient response to treatment using biomarkers, such as procalcitonin, can provide valuable information that informs therapy decisions throughout the course of care. Bringing together diagnostic tools, sepsis protocols, and the principles of antimicrobial stewardship can both improve patient outcomes and help fight antimicrobial resistance.
Recent research suggests that the timing of antibiotic therapy is especially important for patients with septic shock. Additionally, physicians also have to consider that researchers have reported an “association between high mortality rates and an excessive combination of antibiotics and a longer treatment period.” Because of both of those issues, physicians walk a tightrope when treating sepsis patients, so the more information available to support antibiotic decision-making, the better.
A paper published in March 2020 in the journal, Infection & Chemotherapy, explores the balancing act in treating sepsis patients while adhering to good stewardship practices. They note that antibiotic stewardship programs (ASP) are especially important in the ICU because “antibiotic overuse is extensive and the issue of multidrug resistance is increasing.” The authors conclude that, “Implementation of ASP for the balanced use of antibiotics in critically ill patients may protect these patients by reducing the speed of antimicrobial resistance acquisition, preserving the antimicrobial activity of antibiotics, and reducing medical costs,” and that for sepsis, “Appropriate risk assessment, implementation of the latest treatment guidelines, antibiotic de-escalation, and to stop antibiotics in patients without infection are strategies that can be applied for sepsis patients in the ICU.”
Opinions expressed in this article are not necessarily those of bioMérieux, Inc.