by the bioMerieux Connection Editors
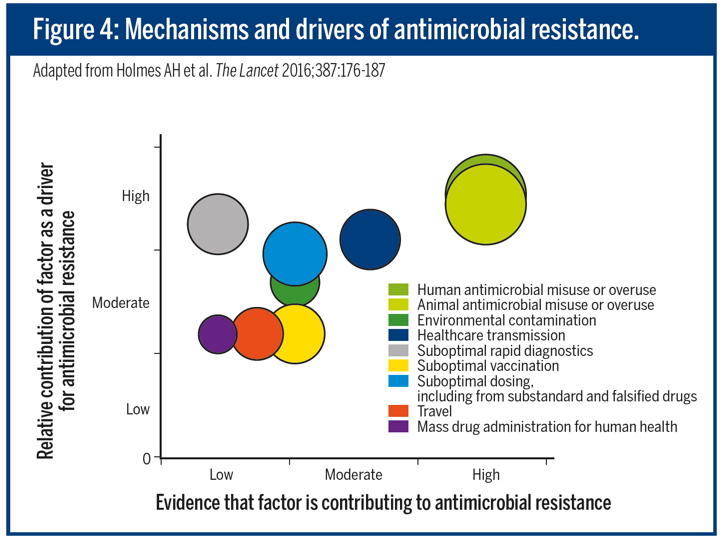
Antimicrobial resistance (AMR) has been identified as a major threat by the World Health Organization due to the lack of new antibiotics in the development pipeline and infections caused by multi-drug resistant pathogens becoming untreatable. There are numerous drivers for AMR. Human antimicrobial misuse and overuse is a key factor, as are suboptimal dosing, lack of availability and/or under-use of rapid diagnostics or point of care tests and insufficient infection prevention and control.
To learn more about the elements of a hospital antimicrobial stewardship program, download the 2019 edition of bioMérieux’s Antimicrobial Stewardship Guide:
Download the Antimicrobial Stewardship Guide For Hospitals
To combat antimicrobial resistance, a three pillar approach is recommended:
- Optimize the use of antimicrobials
- Prevent the transmission of drug-resistant organisms
- Improve environmental decontamination
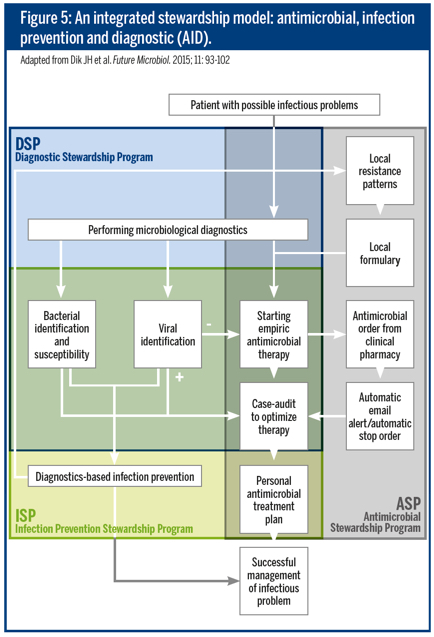
To achieve this integrated approach, antimicrobial stewardship programs (ASPs) have been advocated. This approach encompasses antimicrobial stewardship, diagnostic stewardship, and infection control. The main goals of ASPs are to improve patient outcomes, optimize patient safety, reduce resistance, and control healthcare costs. A number of interventions are key to the success of a hospital-based ASP.
Keys to Success for Implementing an ASP:
1. Assessing motivation
What can be implemented depends on local needs or expertise therefore each hospital’s motivation may differ. Management should analyze their situation, define who they are, define where they want to go, and use quantitative figures while doing so. They should establish a clear vision that is shared by all the stakeholders and conveys a sense of urgency. Stewardship should be a patient safety priority.
2. Accountability and leadership
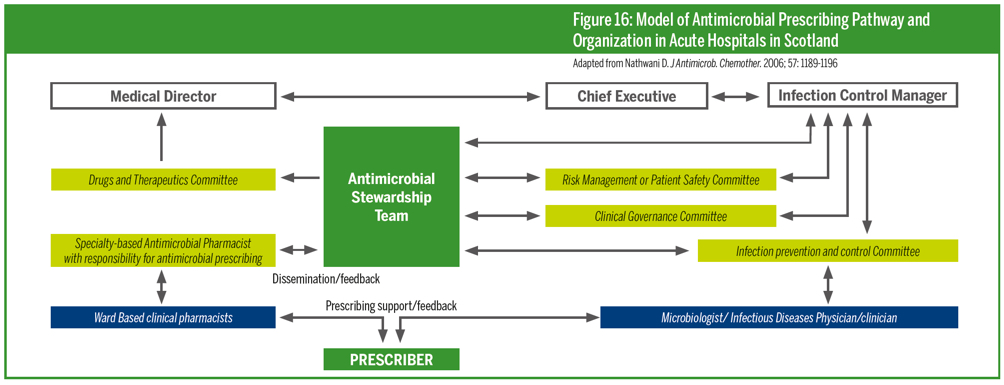
To ensure success, the program should be supported by senior hospital management, and a team of people and resources should be allocated to implement and evaluate the program. ASP team members should possess power, expertise, credibility, and leadership.
3. Structure and organization
Key components of structure are dedicated resources, and a team that includes an infectious disease physician, a clinical microbiologist, and a clinical pharmacist with expertise in infection. The structure should also support clean lines of accountability between those involved.
4. Defining priorities and ways to measure progress and success
ASP objectives should be agreed on by all key stakeholders; this includes how the objectives will be achieved and measured. Plans should include a goal or vision, high level factors that contribute to it, and specific projects that contribute towards each factor.
5. Identifying effective interventions for the setting
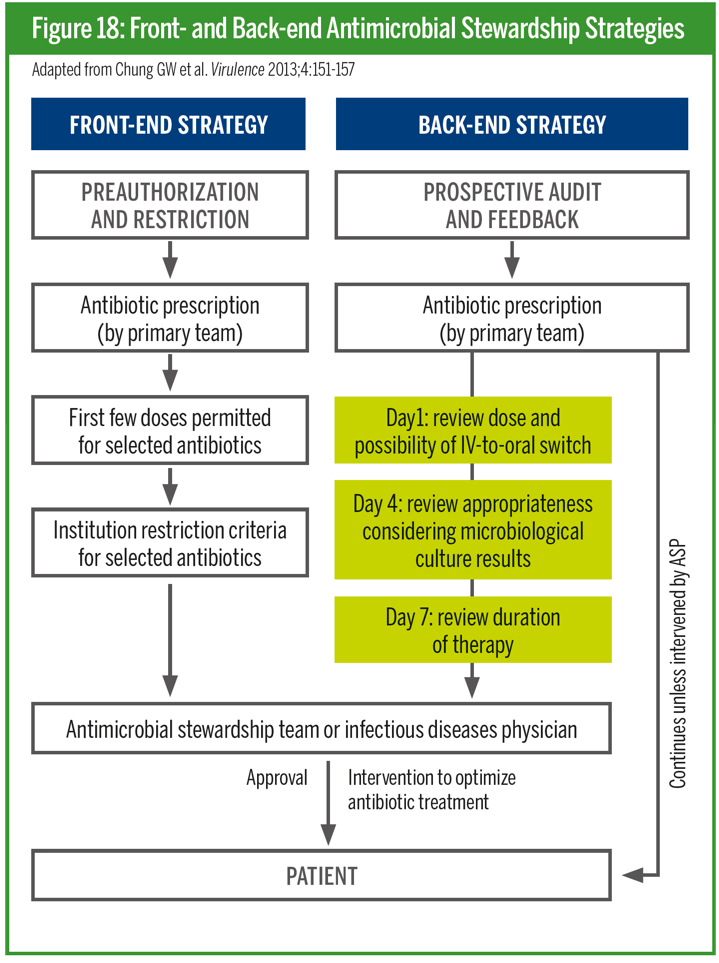
This creates a vision to grow and strengthen the impact of an ASP by identifying supplemental strategies that match the needs of a particular organization. Over time, both front end and back end core strategies have evolved. Learn more about these strategies on page 20 of the downloadable booklet in this article.
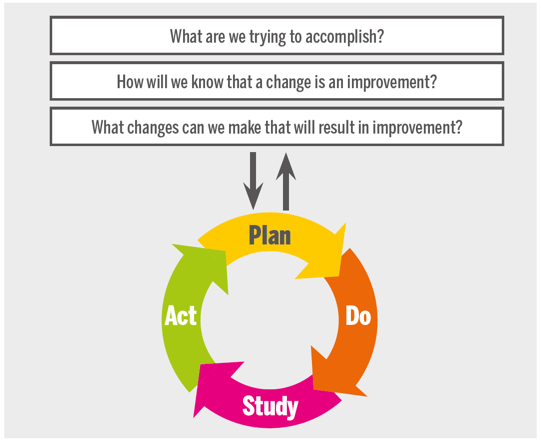
6. Key measurements for improvement
ASPs should establish what to measure, the frequency of measurement, and how the data will be communicated and acted upon. Types of measurement that are commonly used are surveillance of antimicrobial use and resistance, data collection for quality improvement, and analysis of hospital data sets to evaluate consequences of intervention.
7. Education and training
Education is a key component of any ASP. By increasing people’s knowledge and understanding of how antimicrobials should be used to treat common infections and why inappropriate use may lead to resistance and loss of effective treatments, we can protect this valuable resource for future generations.
8. Communication
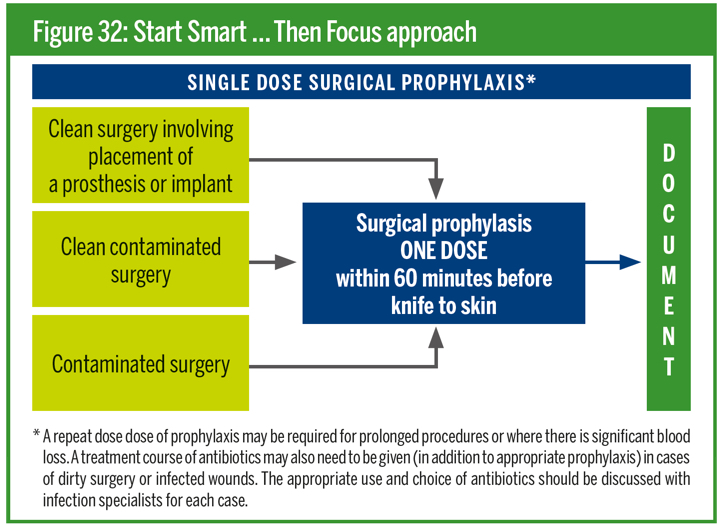
Clear, simple communication should show the vision and the benefits of the program, with core clinical messages. One example of this is the “Start smart – then focus” approach that can be assimilated into practice and provides clear guidelines for antimicrobial use after surgery.
Overall, a number of interventions are key to the success of a hospital-based antimicrobial stewardship program. It is important to ensure early or short-term wins and then to consolidate the success to progress with more innovation. Ensuring all healthcare staff are aware of the importance of stewardship is crucial too, so empower them to act and support.
To learn more about the elements of a hospital antimicrobial stewardship program, download the 2019 edition of bioMérieux’s Antimicrobial Stewardship Guide:
Download the Antimicrobial Stewardship Guide For Hospitals
Opinions expressed in this article are not necessarily those of bioMérieux, Inc.



