Mitigating Global Disparities in the Fight Against Antimicrobial Resistance
By the bioMérieux Editors | Reading time: 4 min
PUBLICATION DATE: MAY 31, 2023
Antibiotics have been used to save countless lives for decades. What happens when these drugs we depend on are no longer effective? Imagine a scenario where routine surgeries and minor infections can frequently become life-threatening, and the cost of treatment increases substantially. It sounds like a bad dream, but the reality is that some people are already experiencing these effects, with some groups and regions more at risk than others.
Impact of Antimicrobial Resistance on Low- and Middle-Income Countries
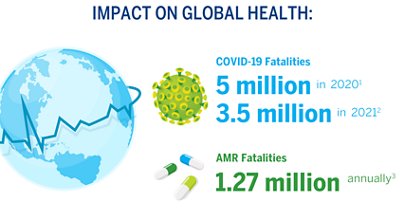
“If we fail to act, we are looking at an almost unthinkable scenario where antibiotics no longer work, and we are cast back into the dark ages of medicine.” stated David Cameron, former UK Prime Minister. Indeed, a recent study in The Lancet estimates that in 2019 alone, 1.27 million deaths were directly attributable to AMR and 4.95 million deaths were associated with bacterial AMR.
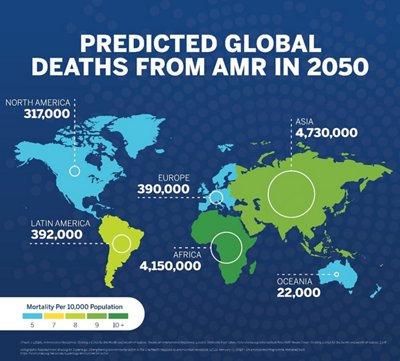
Although AMR is a Global health concern, there are countries and regions that are disproportionately affected. “Low- and middle-income countries bear a greater burden of infectious disease and with limited resources will be most adversely affected by AMR,” states the Technical Brief on Water, Sanitation, Hygiene and Wastewater Management to Prevent Infections and Reduce the Spread of Antimicrobial Resistance. Many low- and middle-income countries (LMICs) lack the infrastructure to adequately prevent and treat infections on a large scale. The lack of organized care, sanitation, hygiene, and clean water contributes to the risk of infection.
A recent GBD (Global Burden of Diseases, Injuries, and Risk Factors) article published regarding the study of The Lancet, provides further insight into the burden of disease in LMICs. Findings indicate that higher income countries, specifically Australasia, had the lowest AMR burden in 2019 with 6.5 deaths per 100,000 attributable to AMR. Consequently, “Western sub-Saharan Africa had the highest burden, with 27.3 deaths per 100,000 attributable to AMR.”
The seriousness of AMR requires a comprehensive, One Health approach to fighting it. As stated by WHO Director-General Tedros Adhanom Ghebreyesus, “[I]t is urgent that nations around the world come together to commit and follow through on the global struggle to stop AMR.”
The tuberculosis example
Tuberculosis (TB) is the 13th leading cause of death worldwide, the second leading infectious killer after COVID-19, and is a major cause of deaths related to antimicrobial resistance. Globally, an estimated 87% of new TB cases were attributed to just eight countries, with the highest mortality rates occurring in the African and South-East Asian regions. In 2019, 465,000 new cases of TB had resistance to rifampicin, the most potent first-line anti-TB drug, of which over three quarters were also resistant to isoniazid (multidrug-resistant TB).
Other types of infections are also burdening healthcare systems worldwide. The Technical Brief notes that, “multidrug-resistant bacteria are carried in the intestinal tract of people and animals around the world, which means untreatable symptomatic infections are challenging health care systems everywhere, rendering antimicrobials less effective.”
Access to Diagnostics is Critical for Addressing AMR
Coordinated action leveraging organizational guidance and support, combined with the appropriate use of rapid clinical diagnostics, can help to make strides against AMR. Rapid diagnostic tests are invaluable in fighting antibiotic resistance because they provide the time-critical information needed to properly identify infection-causing pathogens. That information helps healthcare providers to make appropriate patient treatment decisions and to avoid the misuse and overuse of antimicrobials. Diagnostic tests also contribute surveillance information to track resistance patterns in a healthcare system or region. As emphasized in a recent AMR study, “the need for rapid, highly sensitive, affordable, and cost-effective detection platforms for AMR diagnostics has become urgent.”
Although diagnostic tests have proven to be critical in mitigating infectious disease, global accessibility of these tests has remained an ongoing issue. An article in The Lancet reports that, “…despite diagnostics being central to health care, access to diagnostic testing in pathology and laboratory medicine (PALM) is poor and inequitable in many parts of the world.” While progress has been slow, the WHO’s publication of an essential diagnostics list (EDL) for priority settings in 2018, and the COVID-19 pandemic have both helped to highlight the vital importance of diagnostic tests and accessibility to those tests.
Addressing AMR will take a coordinated global effort that includes individuals at a community level and leaders of nations across the world. Together, we can make progress towards combating AMR for all.
Opinions expressed in this article are not necessarily those of bioMérieux.
You may be interested in these articles
SHARE THIS:
- AMR AMS
< SWIPE FOR MORE ARTICLES >