By the bioMérieux Connection Editors
Explaining science in simple terms can be tough, but for addressing problems like antimicrobial resistance, public awareness and understanding are vital. Here are some common questions and answers.
What is Antimicrobial Resistance? Is it Different from Antibiotic Resistance?
Antimicrobial resistance (AMR) happens when a germ develops or acquires a way to prevent the antimicrobial drug from effectively killing or controlling growth. When germs do not respond to the drugs designed to kill them, infections that used to be treatable can become fatal.
The name, “antimicrobial resistance,” covers all types of germs, more scientifically called microbes, including bacteria, fungi, and viruses, that can cause infections. “Antibiotic resistance” specifically refers to bacteria and does not include other types of germs. Bacteria cause most resistant infections, so the term, “antibiotic resistance” tends to be more common.
Antimicrobial resistance, and more specifically, antibiotic resistance, has become a major threat to our society. Resistance continues to grow because of improper antimicrobial dosage and use. Antibiotics are among the most commonly prescribed drugs used in human medicine and can be lifesaving drugs. But doctors prescribe antibiotics sub-optimally up to half the time, either when not needed or with incorrect dosing or duration.
How Common Are Antimicrobial Resistant Germs?
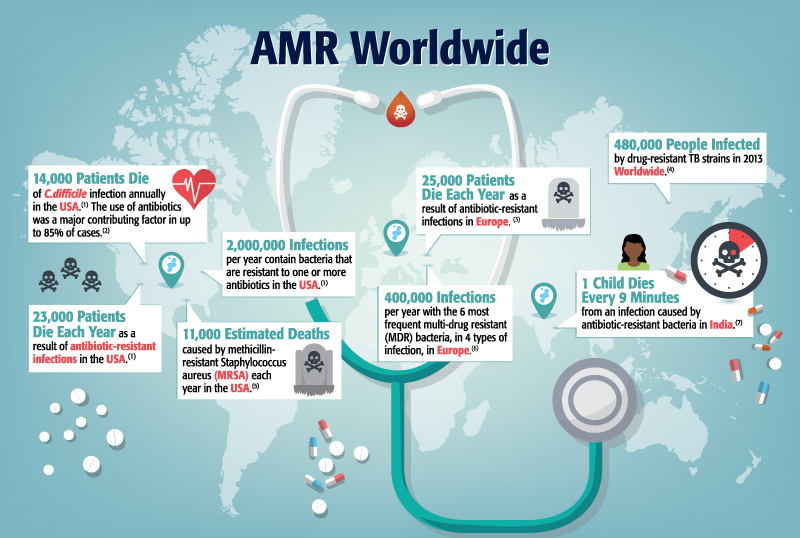
Every year in the United States, at least 2 million people acquire serious infections with multi-drug resistant (MDR) pathogens, and 23,000 of those individuals die as a result.1 Antimicrobial resistance used to be mostly confined to healthcare settings rather than affecting the general community, but over the last 10 years, more drug-resistant infections have arisen within community settings.
By 2050, the Wellcome Trust predicts that resistant infections will be the number one cause of death globally, with an estimated 10 million attributable deaths per year. Considering the limited number of new antimicrobial agents in the pharmaceutical pipeline, we could be faced with challenges that far exceed the current major global illnesses such as HIV, tuberculosis and malaria.
What Else Contributes to Antimicrobial Resistance?
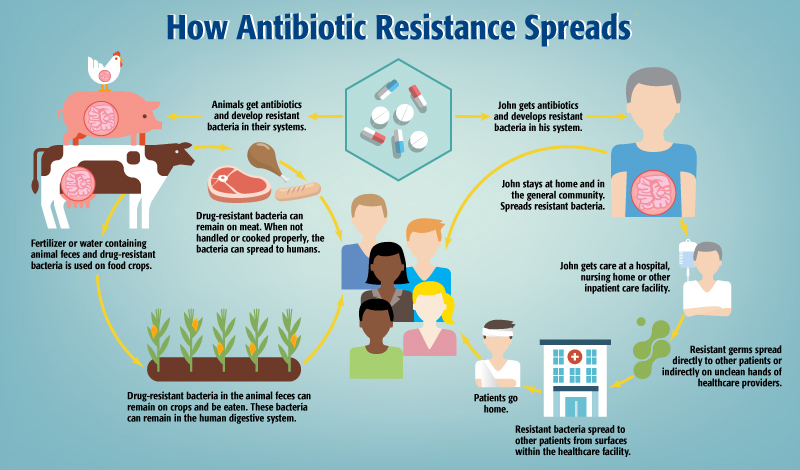
Common food germs like E. Coli and Salmonella become resistant when farms use antimicrobials inappropriately, usually as an attempt to promote animal growth rather than to treat infections. Those resistant infections can spread to humans when we consume contaminated food. To combat the issue, farms should only use antibiotics with veterinary oversight to manage and treat infections, not to promote growth.

How Can We Fight Antimicrobial Resistance?
People can spread resistant bacteria when they don’t use proper hygiene practices, such as washing hands regularly. It’s also important to thoroughly clean surfaces like tables, counters, and doorknobs in homes and especially in public places like schools and restaurants. Healthcare facilities must, and typically do, pay special attention to employee hygiene and thorough environmental sanitation. Finally, healthcare facilities and the food industry must work to reduce improper and sub-optimal antimicrobial use. Implementing Antimicrobial Stewardship Programs (ASPs) paired with rapid diagnostic technologies is a common solution.
Visit Our Resources Page to Download Infographics
Sources:
- Antibiotic Resistance Threats in the United States, 2013. Centers for Disease Control and Prevention (CDC)
- Chang HT et al. Infect Control Hosp Epidemiol. 2007; 28:926-931
- ENVI 2013-04-10 European Report on Patient Safety
- Global Tuberculosis Report. World Health Organization, 2014
- WHO Antimicrobial Resistance Fact Sheet N 194. Updated April 2015.
- Antibiotic Resistance: Implications for Global Health and Novel Intervention Strategies. Washington, DC. The National Academies Press. 2010. (Source ECDC/EMEA 2009)
- Laxminarayan et al. Antibiotic resistance – the need for global solutions. Lancet Infect Dis 2013; 12:1057-98
Opinions expressed in this article are not necessarily those of bioMérieux, Inc.




I will pass this message on to my friends and family
I found this article written for someone who already has an understanding of the topic or has a good medical knowledge base. Even after reading the article twice, what types of illnesses should a antimicrobial be taken and what illnesses are not affected by antimicrobials?
yes my colleagues, are you fine? God bless! i am so fine! your way of presentation is very nice and i would like to appreciate and proceed by this way. And please we need your help to combat AMR. We clinical pharmacists in Ethiopia, siltie zone, Worabe comprehensive specialized hospital wants you to help our motivation to prevent AMR. Let’s combat antimicrobial resistance together!!! yours clinical pharmacist shafi hassen from Ethiopia, siltie zone Worabe comprehensive specialized hospital, Ethiopia